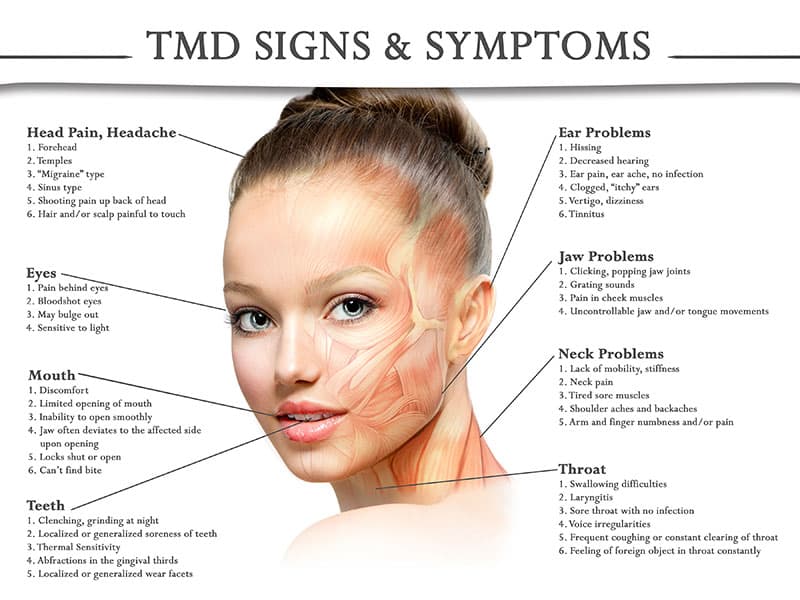
Do you have frequent headaches or migraines, earaches or tinnitus, tender jaw muscles, or a dull aching facial pain? Do you often have neck and shoulder pain? Does your jaw lock or stray to one side when you open your mouth? These aches and pains may be related to the jaw joint, called the temporomandibular joint or “TMJ,” and the muscles that work to move the joint. These painful conditions are often called “TMD” for temporomandibular disorders.
What causes TMD?
The National Institute of Dental and Craniofacial Research classifies TMD by the following:
- Myofascial pain is the most common form of TMD. It results in discomfort or pain in the connective tissue covering the muscles (fascia) and the muscles that control the jaw, neck, and shoulder function.
- Internal derangement of the joint. This means a dislocated jaw or displaced disk. A disk is the cushion of cartilage between the head of the jaw bone and the skull. Or it may indicate an injury to the condyle. This is the rounded end of the jaw bone that articulates with the temporal skull bone.
- Degenerative joint disease is another cause which includes osteoarthritis or rheumatoid arthritis in the jaw joint.
You can have one or more of these conditions at the same time.
What causes TMD?
Several underlying conditions are associated with TMD. This often makes it difficult to pinpoint the cause of a case of TMD. Related conditions may include:
- A jaw or head injuries
- diseases that affect the muscles or joints, such as arthritis
- tooth grinding
- stress
- sleep disorders
How is TMD diagnosed?
A complete evaluation is recommended to determine how best to treat your condition. This will include:
- Health history. Your dentist will ask if you have a history of facial or jaw pain when you chew, bite, or open your mouth. Your provider will ask if you have had cracking, popping, or noise when opening or closing your mouth.
- Physical exam. Your dentist will check if you have facial or jaw pain when moving your jaw or cannot open your mouth wide. He or she will also check for TM joint noises when you open or close your mouth.
- Imaging tests. X-rays, CT scans, MRIs, and models of your teeth to see how your bite fits together, may be used to clarify a diagnosis.
How is TMD treated?
For some patients, the disorders are often managed rather than cured. There are several ways TMD may be managed. The treatment’s success often depends upon you and your dentist working together to find what works to relieve your symptoms.
Treatment may involve a series of steps. The step-by-step plan allows you to try simple treatment before moving on to more involved treatment. As always, our approach is “less is often best.”
The following self-care practices may be recommended:
- Eating softer foods or avoiding foods that cause symptoms
- Minimizing extreme jaw movements, such as yawning, yelling, or singing
- Avoid chewing gum
- Modifying the pain with heat or ice packs
- Practicing relaxation techniques to control jaw tension, such as meditation
If necessary, we may recommend the following to relieve your symptoms:
- Exercises to strengthen jaw muscles
- Medicines to reduce pain or inflammation, or to help you relax
- A night guard or bite appliance to decrease clenching or grinding of teeth
In some cases, your dentist may recommend fixing an uneven bite by adjusting or reshaping some teeth. Orthodontic treatment may also be recommended.